Medicaid is a massive program in the U.S., serving millions of people and distributing hundreds of billions in funding every year. But with that level of scale comes serious risk: fraud and abuse threaten both dollars and lives.
In FY 2024, the country’s Medicaid Fraud Control Units (MFCUs) secured 1,151 convictions, of which 817 were for provider fraud and 334 for patient abuse or neglect. They also recovered roughly $1.4 billion through civil settlements and judgements, and $961 million in criminal recoveries.
This data points to two realities. First, fraud is pervasive and costly. Second, current methods are under enormous strain.
Investigators and prosecutors must wade through fragmented records, medical files, surveillance media, and call logs, all while ensuring legal compliance and protecting sensitive patient data.
To be effective now, agencies need more than storage or a digital filing cabinet. They require intelligence tools that can connect dots, detect patterns, and accelerate investigations. Healthcare date intelligence tools offer that capability. They can analyze data across sources, surface anomalies, and turn raw evidence into actionable insight.
Counting the Cost
Medicaid fraud is not just about financial losses. The money lost to fraudulent claims takes away from programs that should be supporting patients who need care the most. Every diverted dollar represents fewer resources for treatments, medications, and services that improve lives.
The human cost is even more serious. Abuse, neglect, and exploitation of patients in Medicaid-funded facilities cause harm that cannot always be measured in dollars. Families lose trust in the healthcare system, and patients who are already vulnerable face greater risks.
There is also an operational cost. Medicaid Fraud Units and state agencies spend enormous amounts of time handling fragmented evidence. Investigators often work with documents, audio recordings, videos, and billing data scattered across different systems. This slows down investigations, creates backlogs, and makes it harder to build strong, defensible cases.
The scale of these challenges makes it clear that relying on outdated tools and manual methods is not enough. Agencies need intelligence-driven systems that can reduce costs, cut backlogs, and improve both accountability and patient protection.
Why Traditional Methods Fail
Traditional approaches to Medicaid fraud investigations have reached their limits. The sheer volume and variety of evidence overwhelm investigators, and outdated processes slow everything down. Here are the biggest challenges fraud units face today:
Scattered Evidence
Fraud investigations pull data from many sources such as medical charts, billing records, call recordings, surveillance footage, and legal documents. When this evidence is stored in separate systems, investigators spend valuable time trying to connect the pieces.
Manual Review
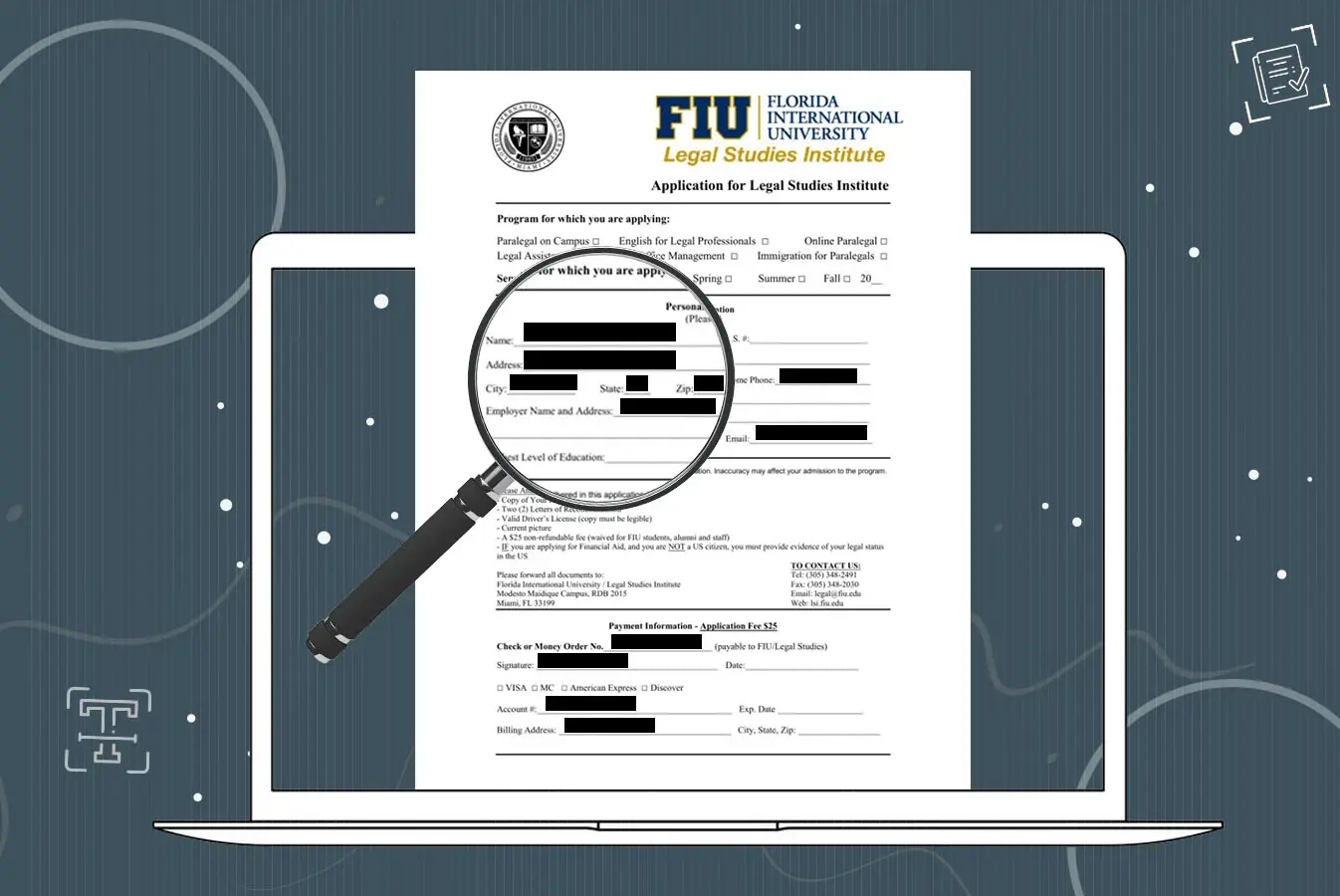
Redacting sensitive patient information is still done line by line or frame by frame in many agencies. This work is slow and prone to human error. Missing even one identifier can jeopardize compliance and weaken a case in court.
Growing Backlogs
Each Medicaid Fraud Unit handles hundreds of cases every year. With so much evidence to analyze, backlogs are inevitable. These delays make it harder to detect fraud early or respond quickly when patients are at risk.
Most existing systems were designed for storing files, not analyzing them. They cannot process the complexity or the volume of modern fraud cases. Agencies need tools that do more than hold evidence.
How Healthcare Data Intelligence Tools Help Fight Medicaid Fraud
Traditional systems can only store files. What agencies need now are tools that analyze, detect, and connect. Healthcare data intelligence tools give Medicaid Fraud Units the ability to work smarter, uncover fraud faster, and protect patients more effectively.
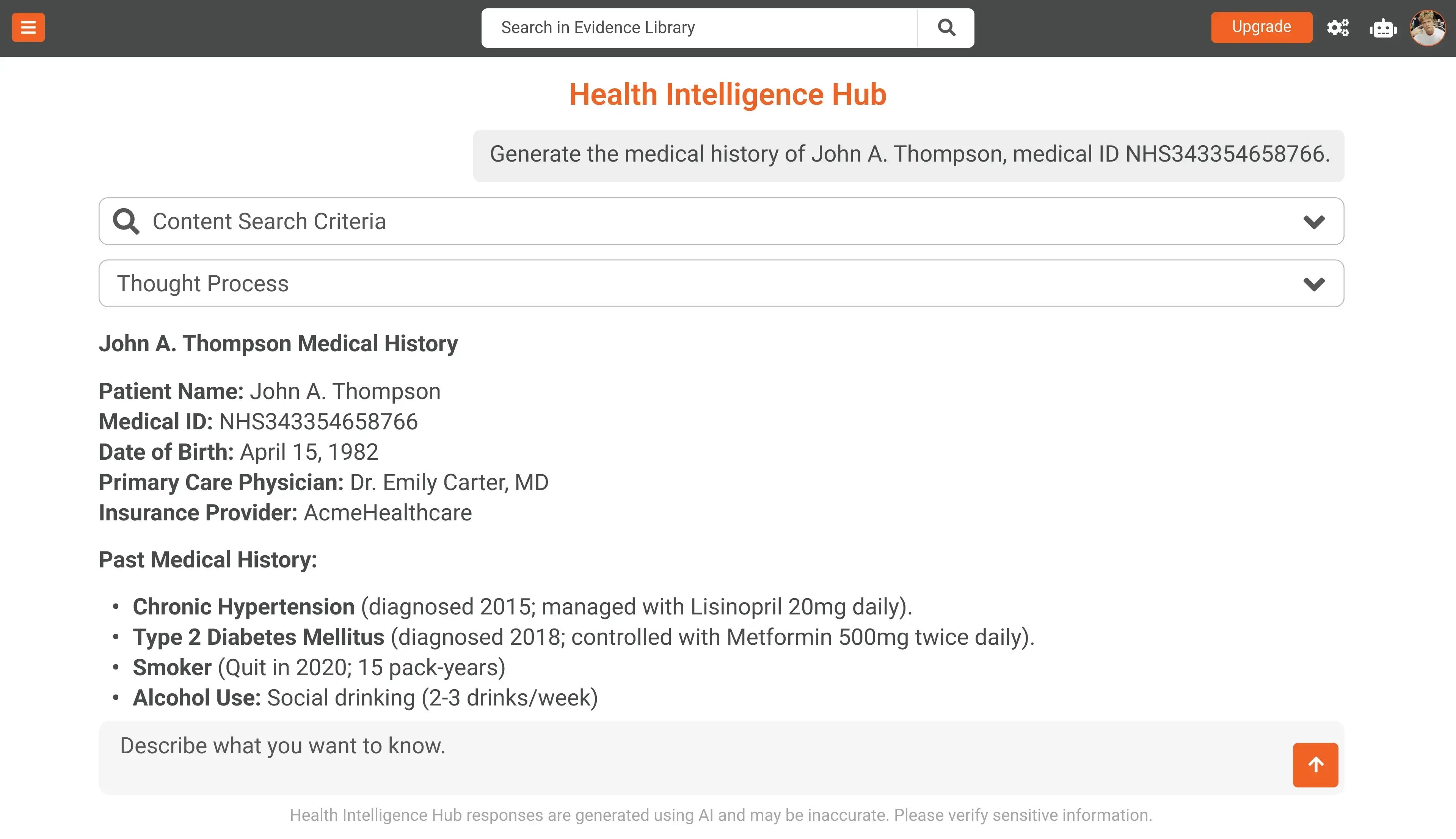
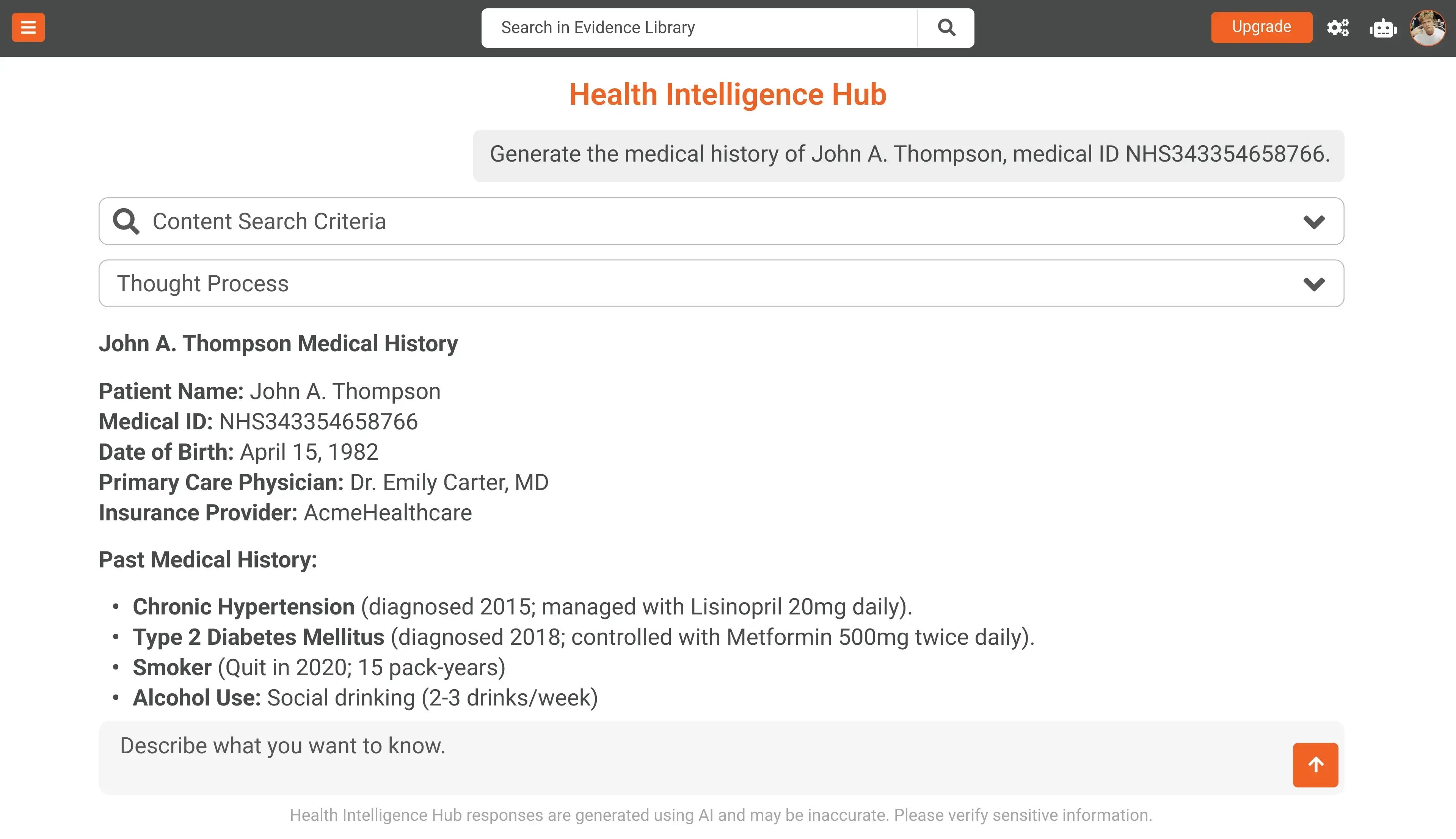
Semantic Search
Instead of digging through endless records, investigators can run simple queries across transcripts, billing data, and medical charts. AI surfaces the most relevant results, making it easier to spot duplicate claims, unusual prescriptions, or repeated provider activity.
Anomaly Detection
AI highlights patterns and outliers that human reviewers might miss. Whether it is billing claims that do not match treatment records or suspicious trends across facilities, anomaly detection acts as an early warning system.
Automated Summaries
Hours of surveillance video, call recordings, or long documents can be condensed into short, clear summaries. Investigators save time, avoid fatigue, and reduce the chance of overlooking key details.
Cross-Case Analysis
Fraud schemes often spread across multiple cases and providers. AI connects dots between records and evidence sources, revealing links that would otherwise remain hidden. This makes it easier to build stronger cases and prevent repeat fraud.
With these capabilities, AI-powered intelligence tools transform the way Medicaid Fraud Units work. Instead of being stuck in manual reviews and backlogs, agencies can focus on recovering funds, holding offenders accountable, and protecting patients.
Benefits for State Agencies
An healthcare data intelligence platform does more than save time. It changes how Medicaid Fraud Units and state agencies approach their work. Here are the key benefits:
Faster Investigations
Automated transcription, translation, and summarization cut review times from hours to minutes. Investigators can spend less time digging through files and more time preparing strong cases.
Better Recovery
Anomaly detection and fraud pattern analysis make it easier to identify suspicious claims early. This means more fraudulent activity is stopped before it escalates, leading to higher fund recovery.
Patient Protection
AI-powered tools help surface evidence of abuse or neglect more quickly. This ensures vulnerable patients are safeguarded sooner and strengthens the cases brought against offenders.
Compliance and Defensibility
With built-in audit trails, chain of custody, and secure redaction of PHI and PII, evidence remains admissible and legally defensible. Agencies can pursue prosecutions with confidence that compliance standards are met.
How VIDIZMO Intelligence Hub Helps
VIDIZMO Intelligence Hub is designed to meet the exact challenges Medicaid Fraud Units face. It is not just a storage system, but a data intelligence platform that turns evidence into actionable intelligence.
Centralized Evidence
All types of evidence can be managed in one place, from medical records and billing data to surveillance video and call recordings. This makes it easier to organize, search, and share information securely.
AI-Powered Insights
The platform uses advanced AI capabilities such as semantic search, anomaly detection, and automated summarization. Investigators can find the right information faster, spot unusual activity, and get concise overviews of complex cases.
Workflow Automation
With no-code workflow design, agencies can build automated processes without relying on IT teams. This allows investigators and attorneys to focus on case strategy while routine tasks are handled by the system.
Compliance and Security
The Intelligence Hub is built to meet strict compliance requirements. It offers encryption, access controls, audit trails, and redaction tools to keep sensitive data secure and ensure evidence remains legally defensible.
By combining AI, automation, and secure evidence management, VIDIZMO Intelligence Hub gives Medicaid Fraud Units the tools they need to investigate smarter, protect patients, and recover funds faster.




No Comments Yet
Let us know what you think