Understanding the HIPAA Privacy Rule for Redaction
by Moazzam Iqbal, Last updated: April 9, 2025, ref:

Do you know that tens of thousands of patient records were posted to the dark web last year?
According to NBC News, hackers published extensive patient data from various hospitals and medical centers. These leaked files contained diagnostic test results, letters to insurers, and personal patient information, putting countless individuals at risk of identity theft and fraud.
This isn’t an isolated incident. Healthcare data breaches are at an all-time high, with 167 million individuals affected in 2023 alone, according to the U.S. Department of Health and Human Services (HHS). Cybercriminals are aggressively targeting electronic health records (EHRs), making data security and redaction more critical than ever.
For healthcare providers, insurers, and business associates, ensuring PHI is redacted before sharing is not just a best practice—it’s a HIPAA compliance requirement. Failure to properly redact sensitive information can result in financial penalties ranging from $100 to $50,000 per violation, with annual caps reaching up to $1.5 million for repeated violations.
In this blog, we’ll break down HIPAA’s redaction rules, explore why PHI redaction is necessary, and introduce an AI-powered HIPAA-compliant redaction solution to help organizations protect patient data effectively.
PHI Under HIPAA Compliance: An Overview
The Health Insurance Portability and Accountability Act (HIPAA) was passed by the U.S. Department of Health and Human Services in 1996 and updated with the HITECH Act in 2009. It provides rules for the privacy and protection of medical records and health information of patients.
All covered entities (health providers, health plans) and business associates who collect patient health information (PHI) are bound to follow the HIPAA rules, which ensure the security of an individual’s health information.
All health information is considered PHI when it includes individual identifiers.
PHI data under HIPAA compliance could be any information in the form of:
- Physical data
- Digital data
- Spoken words
Protected Health Information (PHI) is any health information, including demographic information, which is associated with:
- Past and present physical and mental health conditions of an individual.
- Provision of healthcare to the individual.
- Payments for the provision of healthcare to the individual.
As per HIPAA Privacy Rule, there are 18 identifiers of PHI:
- Name
- Address
- All elements of dates, including birthdates, admission and discharge dates, date of death etc.
- Telephone numbers
- Email addresses
- Fax numbers
- Social Security numbers
- Medical record numbers
- Health Plan Beneficiary numbers
- Account numbers
- Certificate or license numbers
- Vehicle identifiers and serial numbers, including license plate numbers
- Device identifiers and serial numbers
- Web URL
- Internet Protocol IP Address
- Finger or voice print
- Photographic Images (Not limited to Face only)
- Any other characteristic that could uniquely identify the individual
Who is Bound to Follow HIPAA Privacy Rule?
All covered entities (healthcare providers, health plans, and healthcare clearinghouses) and business associates who collect and maintain a record of patient health information (PHI) are bound to follow the HIPAA rules.
HIPAA ensures that an individual’s health information is secured. Covered entities can include a person, organization or any institution. HIPAA Privacy Rule applies to the following covered entities:
.jpg?width=1920&height=1080&name=Blog%20Image-%20Sidra%20(004).jpg)
The breach of the above-mentioned information is considered a HIPAA violation and is a serious crime that results in penalties.
According to American Medical Association,
“Violation of HIPAA compliance rules results in penalties ranging from min $100 to max $50,000 per violation with an annual max of $25,000 for a repeat violation.”
De-identification/Redaction Rules Under HIPAA
PHI must be redacted before being shared with others to prevent violations. Redaction under HIPAA is covered in the Privacy Rule, which regulates the use and disclosure of personal health information.
According to the Privacy Rule of HIPAA, it is termed as ”deidentification,” where you can easily hide one of the 18 identifiers of PHI.
The basic principles of the HIPAA Privacy Rule are as follows:
- The rule protects all PHI, including individually identifiable health or mental health information held or shared by covered entities.
- It limits the conditions under which covered entities may disclose PHI.
- The covered entity is responsible for giving access to individuals with their own PHI.
HIPAA Privacy Rule permits patients and medical professionals to access their medical records for treatment, payment, and health care purposes.
However, this rule does not apply only to healthcare organizations; in fact, sometimes, health records need to be shared with covered entities.
“Covered Entities” include Health plans, healthcare providers, healthcare clearinghouses, business associates, and health insurers. For example, health insurers can gain access to PHI for billing information with patients' consent ensuring that PHI is properly protected.
In certain circumstances, covered entities can use and disclose health information without patients' authorization, which is as follows:
- When required by federal law for public health purposes.
- When required by law enforcement agencies.
- For clinical research purposes.
- Conducting health care operations (quality assurance, compliance monitoring).
- Reporting abuse victims and violence cases.
- Health oversight activities.
- Judicial or administrative matters.
Under the rules and regulations mentioned above, covered entities are held accountable for the proper handling and deidentification of personal information before disclosure. Therefore, redaction is necessary to remove personal health-related information from medical records before sharing.
Redaction is a time-consuming process, so many organizations are looking for efficient HIPAA-compliant redaction Software that saves time.
VIDIZMO: As a HIPAA Compliant Redaction Tool.

Are you looking for a redaction software that is fully compliant with HIPAA Privacy Rule and fulfill all your redaction needs?
Then here is a solution for you!
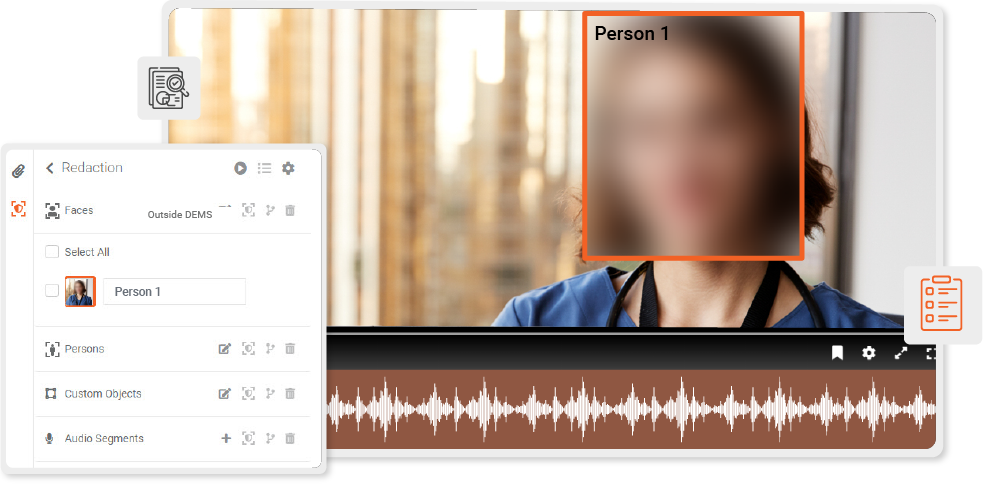
VIDIZMO Redaction is a HIPAA-compliant redaction software that redacts audio recordings and videos highlighting personal health information in medical records using artificial intelligence services.
Key features of the VIDIZMO redaction tool include:
- Detect and track faces and bodies and redact them automatically by using artificial intelligence.
- Blur objects in images, mute or bleep audio segments, and hide specific words in documents containing PHI.
- Hide sensitive PHI appearing in videos, such as names, medical records, full-face photos, etc.
- Redact multiple files simultaneously.
- AI-Powered redaction with manual redaction capabilities for accurate results.
- It has an IDC-recognized Digital Evidence Management System* with a chain of custody, transcription, translation, and secure sharing features.
It also offers a HIPAA-Compliant Video Platform with various security features to protect PHI.
Final Thoughts: Ensuring HIPAA Compliance with AI-Powered Redaction
Protecting Protected Health Information (PHI) is a legal and ethical responsibility for healthcare organizations. With HIPAA violations leading to severe penalties, ensuring proper redaction of medical records before sharing is essential. The HIPAA Privacy Rule mandates strict control over PHI redaction, helping organizations prevent data breaches and unauthorized disclosures.
By leveraging AI-powered redaction tools, healthcare providers can automate PHI redaction, ensuring compliance with HIPAA redaction requirements while saving time and resources. VIDIZMO’s HIPAA-compliant redaction software enables seamless redaction of PHI in videos, audio, and documents, ensuring privacy, security, and regulatory compliance.
Start your 7-day Free Trial today and experience AI-driven PHI redaction with VIDIZMO!
People Also Ask
What is HIPAA redaction, and why is it important?
HIPAA redaction is the process of removing or obscuring Protected Health Information (PHI) from medical records to prevent unauthorized access. It is essential because HIPAA compliance requires organizations to protect patient data from breaches, identity theft, and legal violations.
What information needs to be redacted for HIPAA compliance?
Under the HIPAA Privacy Rule, 18 PHI identifiers must be redacted or de-identified before sharing medical records. These include patient names, Social Security numbers, medical record numbers, addresses, phone numbers, and biometric data to prevent unauthorized identification.
How does HIPAA-compliant redaction work?
HIPAA-compliant redaction automatically detects and removes PHI from text, images, videos, and audio files. Advanced AI-powered redaction tools can identify faces, medical record numbers, and spoken patient names, ensuring compliance with HIPAA redaction requirements while preserving document usability.
Who is required to follow HIPAA redaction rules?
All covered entities (healthcare providers, insurers, and healthcare clearinghouses) and business associates (third-party vendors handling PHI) must follow HIPAA redaction requirements to avoid compliance violations and penalties.
What is the penalty for failing to redact PHI under HIPAA?
Failing to redact sensitive PHI can result in HIPAA violations, with fines ranging from $100 to $50,000 per violation and an annual cap of $1.5 million for repeated offenses (HIPAA Journal).
What is the difference between redaction and de-identification in HIPAA?
Redaction is the removal or obscuring of PHI to prevent unauthorized access, while de-identification ensures PHI is modified so it cannot be traced back to a specific individual. HIPAA allows two de-identification methods: Safe Harbor and Expert Determination.
Can AI software help with HIPAA-compliant redaction?
Yes, AI-powered redaction software like VIDIZMO automates PHI redaction by detecting and blurring sensitive data in videos, audio, and text documents. This ensures efficient, accurate, and HIPAA-compliant redaction with minimal manual effort.
What types of medical records need redaction under HIPAA?
Medical records that contain patient-identifiable information—including doctor’s notes, prescriptions, diagnostic test results, and insurance claim documents—must be redacted before being shared with unauthorized parties.
Does HIPAA require redaction in video and audio recordings?
Yes, HIPAA compliance applies to video and audio recordings that contain PHI identifiers, such as spoken names, medical record numbers, and patient details. AI-based redaction tools can mute, bleep, or blur PHI in recordings to meet compliance standards.
How can I ensure my organization complies with HIPAA redaction rules?
To comply with HIPAA redaction requirements, organizations should:
- Implement AI-powered PHI redaction software
- Follow the Safe Harbor or Expert Determination de-identification methods
- Regularly audit and update redaction processes
- Train employees on HIPAA compliance and PHI security
Jump to
You May Also Like
These Related Stories

Ensure Data Privacy and Compliance with Bulk Audio Redaction Software
Redaction Software Implementation Best Practices for Federal Agencies


No Comments Yet
Let us know what you think